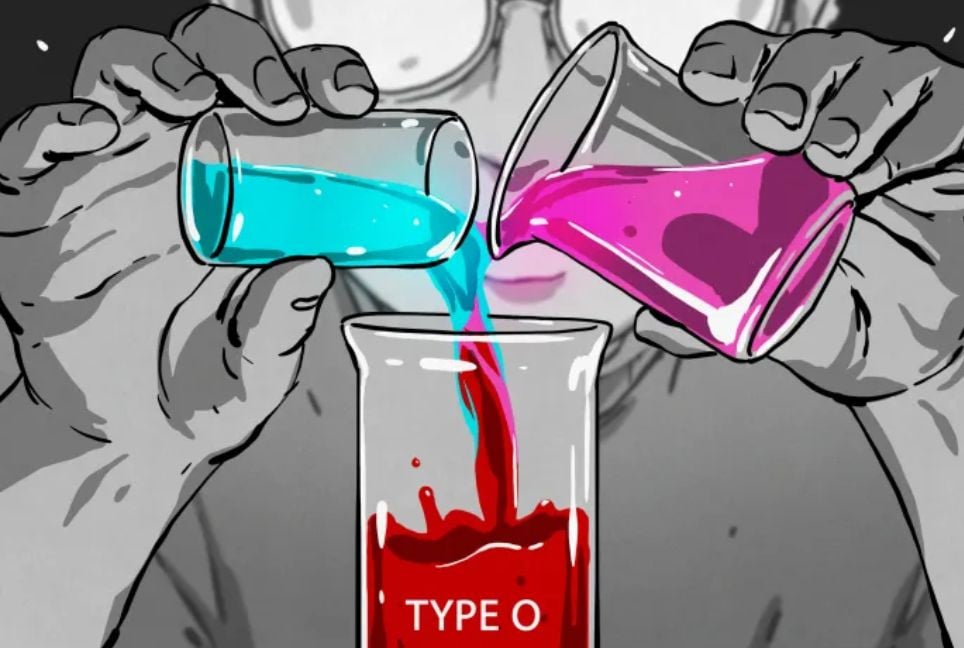
Scientists are advancing in the development of artificial blood to address global blood shortages.
Millions die annually due to the lack of access to safe blood transfusions. Artificial blood, which can be lab-grown or synthetic, could improve emergency medicine, surgeries, and transfusions.
What is artificial blood?
Artificial blood includes both lab-grown and synthetic blood. Synthetic blood is a fully man-made substitute that mimics blood cells' oxygen-transporting function, mainly for emergency use where blood matching is difficult.
The U.S. military has invested $46 million in ErythroMer, a synthetic blood substitute. Meanwhile, lab-grown blood involves cultivating human red blood cells in controlled environments. It could improve treatment efficacy, such as using lab-grown platelets for trauma patients.
How is lab-grown blood made?
Lab-grown blood starts with stem cells, which can develop into red blood cells, platelets, or other cell types. Haematopoietic stem cells from bone marrow or blood are used to create red blood cells.
In the lab, these cells are exposed to growth factors, allowing them to mature into functional red blood cells. Genetic editing may help remove blood group markers, creating universal blood that doesn’t require matching blood types.
How close are scientists to producing artificial blood?
Both lab-grown and synthetic blood products are still in research stages. A 2022 clinical trial in the UK tested lab-grown red blood cells in humans. While production costs have decreased significantly, lab-grown blood is still much more expensive than donated blood. Further trials are needed for safety and approval.
Has artificial blood been used in clinical trials?
Yes, a 2022 trial in Japan tested haemoglobin vesicles, artificial components that carry oxygen like red blood cells. The study found mild side effects but no significant vital sign changes, showing potential as a blood transfusion alternative.
How far are we from manufacturing blood commercially?
Challenges in scaling production to meet clinical demand remain. Regulators are also uncertain about how to classify and regulate artificial blood, creating unknowns in its commercialization.
Can artificial blood be made for rare blood groups?
Yes, lab-grown blood can be tailored for rare blood types, and synthetic blood can be universal due to its lack of blood group markers, making it an alternative for transfusions.
Could artificial blood solve global blood shortages?
Artificial blood could address blood shortages, especially in low- and middle-income countries, where storage and access are major challenges. Lab-grown blood could provide a solution for crisis situations, such as natural disasters or pandemics, ensuring more people receive lifesaving transfusions.
Source: Al Jazeera
Bd-pratidin English/FNC